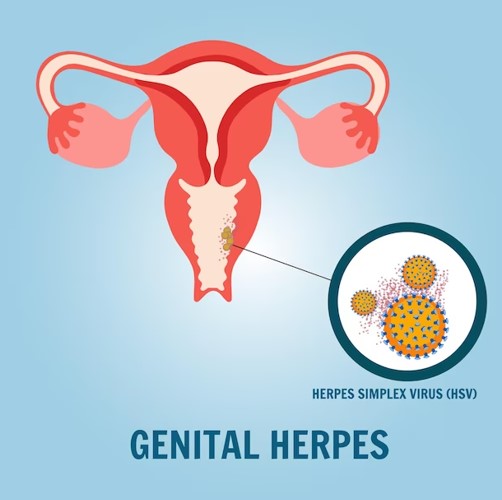
The Contagious Nature of Genital Herpes
Picture a flare-up of painful blisters. Genital herpes is most contagious during these active outbreaks. The fluid from the sores teems with the virus, making contact highly risky.
However, the virus doesn’t always need visible sores to spread. Asymptomatic shedding means the virus can be on the skin’s surface even without symptoms, silently passing from one person to another. This silent spread is the reason why regular testing and open communication are so vital.
Oral to genital transmission is another concern. Oral herpes (HSV-1) can be transmitted to the genital area through oral-genital contact. It’s a reminder that protection, like dental dams, should be considered during oral sex.
Suppressive therapy offers hope for those with frequent outbreaks. Daily antiviral medication can reduce viral shedding and lower the risk of transmission, allowing couples to maintain their intimacy with less fear.
After a genital herpes diagnosis, several common concerns and threats may arise:
1. Transmission to Partners:
The risk of spreading the virus to sexual partners becomes a major concern. Effective communication and using protection like condoms are crucial to minimize this risk.
2. Stigma and Judgement:
There is often a significant emotional burden due to the stigma associated with sexually transmitted infections (STIs). Fear of judgment from partners, friends, or family can lead to feelings of shame and isolation.
3. Recurring Outbreaks:
Worries about the frequency and severity of herpes outbreaks are common. Many fear the pain, discomfort, and inconvenience associated with recurring sores.
4. Impact on Relationships:
Concerns about how the diagnosis will affect current and future relationships can be distressing. There is anxiety about having to disclose the condition to potential partners and the fear of rejection.
5. Complications During Pregnancy:
For those who are pregnant or planning to become pregnant, there is concern about transmitting the virus to the baby during childbirth. This can lead to stress and the need for medical intervention.
6. Emotional and Mental Health:
The diagnosis can lead to anxiety, depression, and a decreased sense of self-worth. The emotional impact can be significant and may require professional support or counselling.
7. Managing Symptoms:
Learning to manage symptoms and prevent outbreaks through medication and lifestyle changes becomes a priority. Concerns about the effectiveness of treatment and side effects of medications are also common.
8. Social and Work Life:
There might be concerns about how the condition could affect social interactions and professional life, especially during outbreaks.
9. Long-term Health:
Though serious long-term health complications are rare, worries about the potential for increased risk of other STIs and general health can be unsettling.
Dermatologist Intervention
When dealing with recurrent or severe outbreaks, seeking the advice of a dermatologist can be invaluable. Dermatologists specialize in skin conditions, including genital herpes, and can offer tailored treatment plans to help manage the condition effectively. For instance, a dermatologist can:
1. Prescribe Antiviral Medication: Beyond the standard antiviral treatments, dermatologists might suggest specific dosages or combinations based on individual needs.
2. Provide Pain Relief Strategies: They can recommend topical treatments or other pain relief methods to help alleviate the discomfort during outbreaks.
3. Monitor and Manage Symptoms: Regular check-ups with a dermatologist can help track the frequency and severity of outbreaks, allowing for adjustments in treatment as needed.
4. Offer Support and Guidance: Dermatologists can provide valuable information on lifestyle changes, stress management techniques, and other factors that can influence the frequency of herpes outbreaks.
Living with Genital Herpes
Receiving a genital herpes diagnosis can feel like a storm cloud has settled over your life. But it’s a manageable condition. Antiviral medications can help control outbreaks, and over-the-counter pain relievers can ease the discomfort during flare-ups.
The emotional toll can be significant. Imagine feeling isolated or ashamed. Seeking support from healthcare professionals, support groups, or counselors can provide much-needed comfort and guidance.
Living a healthy lifestyle can also make a difference. Regular exercise, a balanced diet, and stress management can boost your immune system, potentially reducing the frequency of outbreaks.
Conclusion
Genital herpes is more than just a physical condition; it’s a journey that many people navigate daily. Understanding its causes, practicing prevention, and recognizing its contagious nature are crucial steps in managing and reducing its spread. By fostering awareness and encouraging open communication, we can combat the stigma associated with genital herpes and support those affected by it. Knowledge is power, and being informed is the first step toward prevention and effective management.
If you have questions or concerns about genital herpes, consulting a healthcare professional is the best way to get personalized advice and support.
ABOUT THE AUTHOR -
She is a renowned MD Dermatologist with over 10 years of experience & has dedicated their career to understanding the complexities of skin health.
She diagnoses and treats dermatology conditions affecting the skin, hair, scalp, mouth, nails, and genitals.
She diagnoses and treats the patients at Fabderma Clinic, which is owned by herself and a leading medical and cosmetic dermatology clinic situated in Thane where a range of dermatology conditions are treated with the highest level of comfort.
She combines cutting-edge research with a commitment to transparency, ensuring that you understand exactly what you're putting on your skin.